
Pharmacy Closures Are a Prescription for Catastrophe
As national retail pharmacy chains collectively shutter thousands of locations nationwide, NYITCOM Associate Professor Maria Pino, Ph.D., explains the potential impact on Long Island, where more than a dozen Rite Aid stores have already disappeared.
This October, just in time for flu season, Walgreens announced plans to close 1,200 stores nationwide. The news came on the heels of CVS closing 900 locations and Rite Aid shuttering hundreds of its own.
On Long Island, more than a dozen Rite Aid stores closed, including those in Floral Park, Levittown, Bay Shore, and Huntington Station, among others.
If you think a pharmacy desert could never happen here, think again.
Pharmacy deserts, defined as areas lacking convenient access to a pharmacy, make it harder for patients to obtain necessary medications and preventative vaccines. While this might conjure images of far-off, remote communities, pharmacy deserts can emerge in densely occupied areas. In fact, a 2022 study by Yale and Cornell University researchers uncovered a total of 670 in New York City, Chicago, and Los Angeles.
When the neighborhood drugstore closes, patrons lose more than access to medications; they lose the vital expertise of pharmacists. This is especially concerning because pharmacists, with whom no appointment is necessary, are among the most accessible healthcare professionals in many communities. Some patients with chronic conditions may also halt medication regimens. For those with hypertension, diabetes, asthma, and heart disease, this could spell serious complications—even death.
One population we must consider is the elderly, a group that accounts for up to 30 percent of prescription medications in the United States. Driving farther to access their prescriptions is not an option for many of these individuals, who are also at higher risk for adverse reactions, drug interactions, and medication errors. In addition, patients with mental health conditions may struggle. If unable to adhere to their treatment plans, they could face suicide, unemployment, and homelessness.
Pharmacy deserts also have financial implications. Nonadherence, when a patient fails to follow a prescribed treatment plan, is a main source of healthcare system waste, with avoidable hospitalizations costing the United States approximately $100 billion annually. When national healthcare costs rise, so too do Medicare and Medicaid expenses, which are funded by taxpayer dollars. And, when more patients are unable to stick to their treatments, they will use additional sick days and disability, leaving employers less productive and less profitable.
Lastly, as the pandemic has shown, vaccines are critical to maintaining a normal, functioning society. But, when getting vaccinated now requires a commute, people will forego the recommended flu, COVID-19, pneumonia, and RSV shots. As such, transmissible diseases will spread more easily, infect vulnerable populations, disrupt the workforce, and restrict social gatherings, among other consequences.
Thankfully, Long Islanders have a few resources at their disposal. Many insurance plans allow physicians to prescribe a 90-day supply for chronic conditions, which can be sent directly to the patient’s home. Some patients will, undoubtedly, turn to online pharmacies. But those who are less tech-savvy or unable to drive should inquire about delivery and shipping options at the closest pharmacy, which may offer “refill by phone” options. In addition, some healthcare clinics and medical schools, like the one at which I teach, often provide vaccination services.
There are also steps that pharmacies can take. Drugstore representatives should lobby New York State officials to pass Assembly Bill a7592, which would permit telepharmacy throughout the state. Telepharmacy, which is already offered in 29 other states, provides patients with video call access to a pharmacist or supervised technician, who can verify prescriptions and counsel the patient remotely. In addition, pharmacies now managing the needs of broader geographic areas and more diverse populations should employ bilingual staff to ensure that all patients have an equal opportunity to fully understand their medications.
Pharmacy deserts are a script for public health disasters. Thankfully, for now, we have a few tools that can help us navigate this conundrum.
This article previously appeared in Long Island Business News.
More News
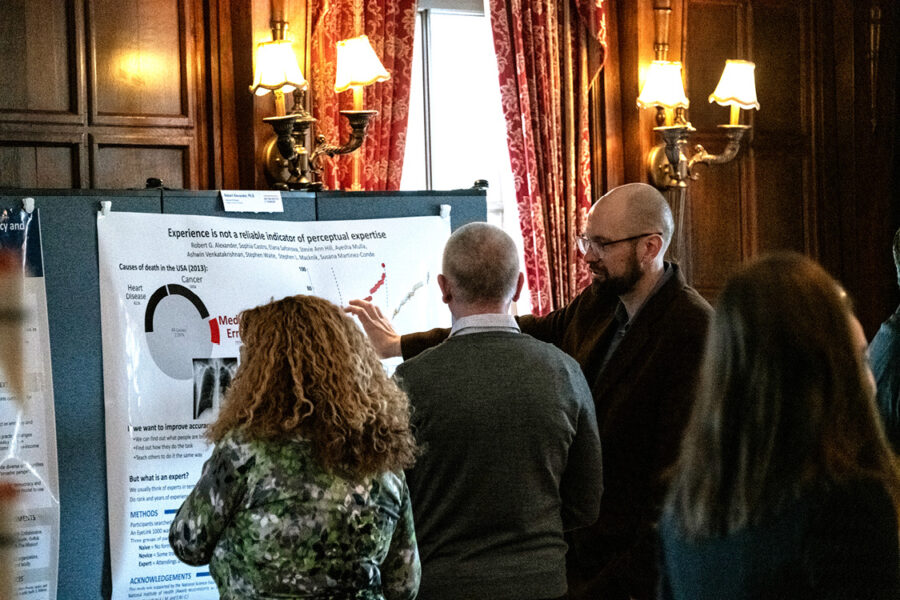
Celebrating Faculty Scholars
Exhibits at the Faculty Scholars Reception showcased faculty and staff’s scholarly and creative achievements during the previous calendar year.

Medical Student Studies Cancer With Catholic Health Physician
Osteopathic medicine/academic medicine (D.O./M.S.) student Rachel Radigan recently completed research on circulating cancer tumor DNA with a radiation oncologist from Good Samaritan University Hospital.
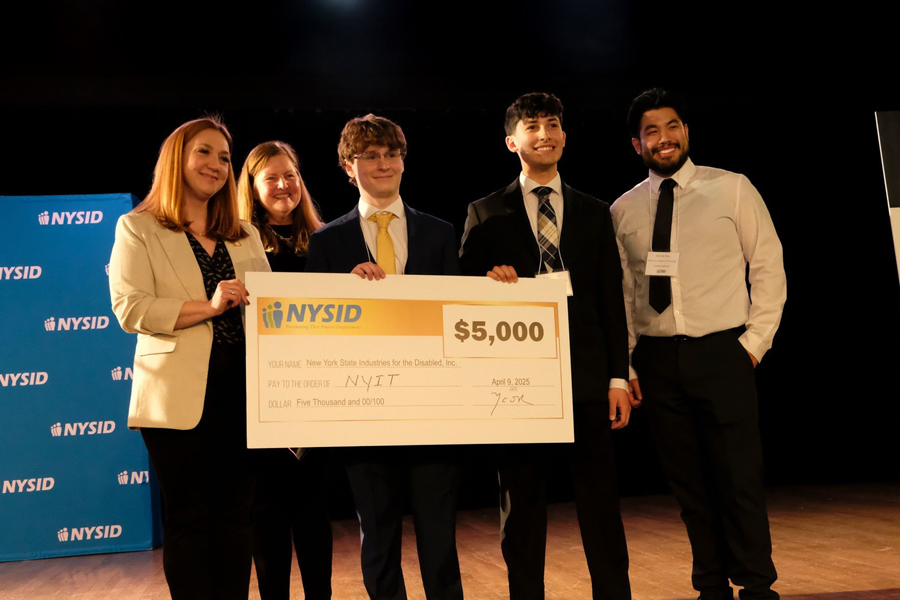
Engineering Students Receive Prize at CREATE Symposium
College of Engineering and Computing Sciences students took home a third-place win for their invention designed to assist those with disabilities in their everyday work tasks.

Leaders in Medicine to be Honored at 2025 Commencement
Two physicians whose contributions to osteopathic medicine have advanced the profession and profoundly impacted the lives of countless others will receive honorary degrees on May 18.

Future Forecast
M.B.A. student Yogesh Singh Katoch hones forecasting models for stock prices, housing prices, and much more.

New Chemistry Offering Joins Ranks of Ph.D. Programs
A Ph.D. in Chemistry will launch in fall 2025, marking the latest entry in the ranks of Ph.D. programs offered at the university.